
Global Oral Health Workforce Survey: Understanding the Landscape
Global Oral Health Workforce Survey: Understanding the LandscapeThe Oral Health Working Group (OHWG) of the World Federation of Public Health Associations (WFPHA) in collaboration with the International Federation of Dental Hygienists and the Seoul...
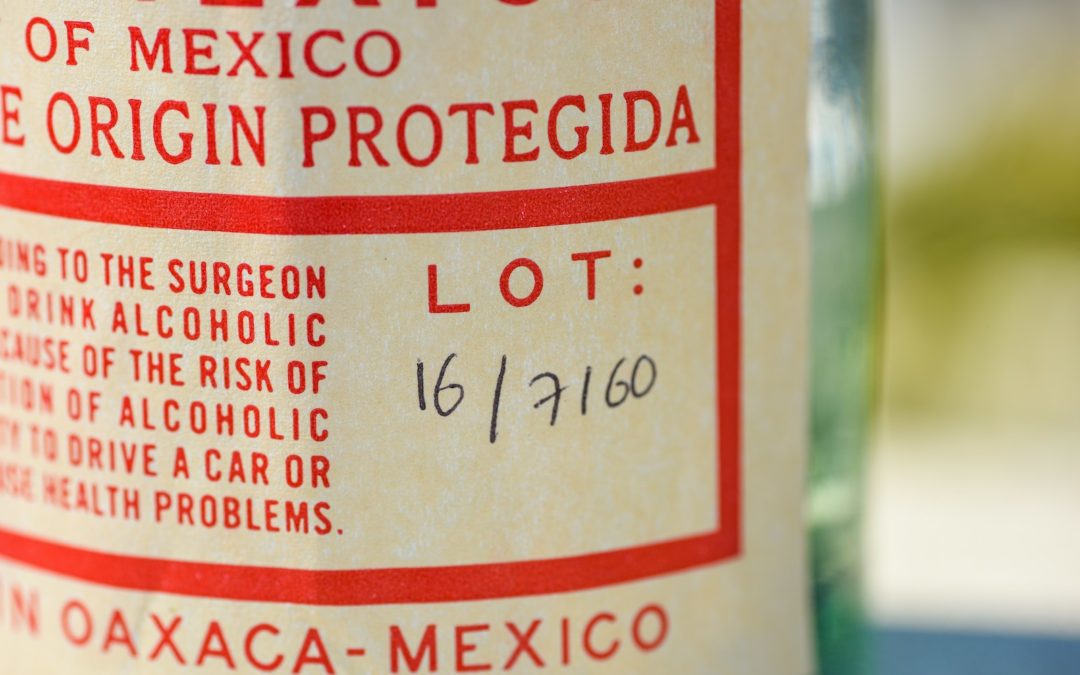
Addressing Alcohol Consumption Through Informed Choices: WFPHA’s Response to Codex’s Call for Comments on Alcoholic Beverage Labeling
Addressing Alcohol Consumption Through Informed Choices: WFPHA's Response to Codex's Call for Comments on Alcoholic Beverage LabelingThe World Federation of Public Health Associations (WFPHA) has recently submitted its comments in response to the...

Empowering Indigenous Voices: Reflections from the Permanent Forum on Indigenous Issues”
Empowering Indigenous Voices: Reflections from the Permanent Forum on Indigenous IssuesPresident-Elect Emma Rawson Te-Patu of the World Federation of Public Health Associations joins a diverse cohort of Indigenous leaders this week at the Permanent...

