
Prof. Ulrich Laaser’s Inspiring Speech at the WFPHA Awards Ceremony 2023

Prof. Ulrich Laaser’s Inspiring Speech at the WFPHA Awards Ceremony 2023
News
May 19, 2023
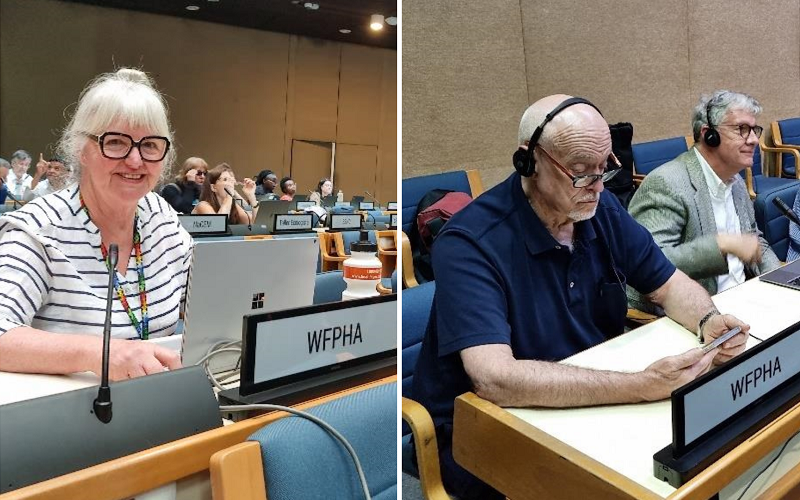
The World Federation of Public Health Associations (WFPHA) recognizes outstanding contributions to public health through its annual awards program. The program aims to acknowledge and honor individuals and organizations that have made significant achievements in promoting health, preventing diseases and injuries, and ensuring safe and healthy conditions for people around the world.
This year, the WFPHA presents a series of awards during the 17th World Congress on Public Health (WCPH), held in Rome, Italy, on May 02 to 06, 2023.
One of the recipients of this year’s awards was Prof. Ulrich Laaser, who received the Lifetime Achievement Award for Excellence in Global Health. Prof. Laaser’s speech during the award ceremony was a captivating and inspirational moment, encapsulating his lifetime of dedication to global health and social justice. His words served as a reminder of the urgent need to work collaboratively, embrace equity, and address the pressing challenges facing our planet. As the public health community moves forward, Prof. Laaser’s legacy will continue to inspire future generations to strive for a healthier and more equitable world.
Prof. Laaser’s speech is available to read here.





Recent Comments